In the high-stakes world of emergency medicine, where every second can mean the difference between life and death, a new innovation from researchers at UC Santa Barbara is turning heads with its potential to transform airway management. Endotracheal intubation, a vital procedure to secure a patient’s airway during critical situations like surgeries or trauma, remains one of the most challenging skills for medical professionals to master. Traditional tools, often rigid and unforgiving, can lead to catastrophic errors under pressure—such as placing the tube in the esophagus instead of the trachea, diverting oxygen to the wrong place. With millions of these procedures performed annually in unpredictable environments, the need for a safer, more reliable solution is undeniable. This article explores a groundbreaking development in soft robotics that could redefine how clinicians approach this life-saving task, making it more accessible and less prone to error even in the most chaotic settings.
Addressing the Perils of Airway Management
Navigating the Risks of Conventional Methods
Endotracheal intubation is a delicate dance between precision and urgency, complicated by the human body’s natural barriers like the epiglottis, a protective flap over the trachea. Clinicians must use stiff instruments, such as metal laryngoscopes, to bypass this defense and insert a breathing tube, often applying considerable force to sensitive tissues. The margin for error is razor-thin; a misplaced tube can send oxygen into the stomach instead of the lungs, leading to fatal consequences. This risk is magnified in emergency scenarios—think roadside accidents or dimly lit field hospitals—where even experienced practitioners can struggle. The inherent limitations of current tools highlight a pressing demand for innovation that prioritizes both safety and ease under less-than-ideal conditions, ensuring that airway access doesn’t become a gamble with lives on the line.
The Toll of Errors in High-Pressure Settings
Beyond the technical challenges, the psychological and environmental pressures of emergency intubation compound the difficulty of the procedure. Medical personnel often perform this task amidst chaos, with limited visibility, noisy surroundings, or inadequate equipment, particularly in remote or underserved areas. Studies show that failure rates for first attempts can be alarmingly high outside controlled hospital environments, leading to prolonged oxygen deprivation and heightened risk of brain damage or death for patients. Compounding this issue is the extensive training required to achieve proficiency with traditional tools, a barrier that excludes many frontline responders from confidently executing the procedure. A solution that simplifies this process could bridge a critical gap, empowering a broader range of healthcare providers to act swiftly and effectively when every moment counts.
A New Frontier in Medical Technology
Unveiling the Soft Robotic Intubation System
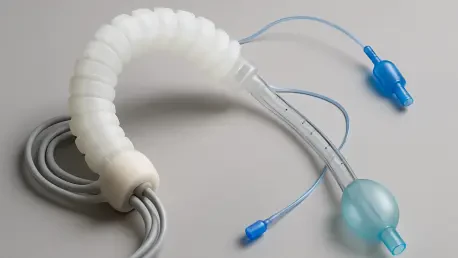
Enter the Soft Robotic Intubation System (SRIS), a pioneering device developed at UC Santa Barbara that challenges the status quo of airway management. Unlike the rigid tools of the past, SRIS utilizes soft, inflatable materials that mimic natural, fluid motion through an innovative “everting” mechanism—essentially, the tube turns inside out as it extends, guiding itself into the trachea with minimal resistance. A curved introducer positions the device at the back of the throat, and from there, the soft tube advances autonomously, adapting to the airway’s unique contours without the need for forceful manipulation. This design, championed by mechanical engineering professor Elliot Hawkes and recent Ph.D. graduate David Haggerty, significantly lowers the risk of trauma to delicate tissues, offering a gentler alternative that could redefine how clinicians secure airways in critical situations.
Advantages of Flexibility Over Rigidity
The core strength of SRIS lies in its ability to adapt to the anatomical variations found across diverse patient populations, a feat traditional rigid tools often fail to achieve. Conventional methods depend on stiffness to push through the airway, frequently resulting in unintended pressure on vulnerable structures and increasing the likelihood of injury. In contrast, the soft robotic approach prioritizes flexibility, allowing the tube to follow the body’s natural pathways with precision and care. This not only enhances safety but also boosts reliability, as the system can accommodate subtle differences in throat and tracheal structures without requiring excessive force. Experts behind the project emphasize that this shift away from a brute-force mentality could set a new standard for medical devices, particularly in scenarios where patient safety hangs in the balance and every movement must be calculated.
Performance Metrics and Real-World Promise
Stellar Outcomes from Initial Testing
Testing of the Soft Robotic Intubation System has produced results that are nothing short of remarkable, showcasing its potential to transform emergency care. Conducted on mannequins and cadavers, trials revealed a 100% success rate among expert users, demonstrating the device’s precision in skilled hands. Even more striking is the performance among non-experts, such as emergency medical technicians, who achieved a 96% success rate after just five minutes of training. An 87% first-pass success rate—meaning correct tube placement on the initial attempt—was recorded among these minimally trained individuals, a statistic that underscores the system’s intuitive design. Perhaps most critical for emergency contexts, non-experts completed the procedure in an average of 21 seconds, less than half the time required by current leading methods like video laryngoscopy, proving that speed and accuracy can coexist.
Breaking Down Barriers to Skill Acquisition
The implications of these test results extend far beyond numbers, pointing to a democratization of a once highly specialized skill. Intubation traditionally demands years of rigorous training, limiting its mastery to a small subset of medical professionals. SRIS, however, slashes this learning curve dramatically, enabling frontline responders with minimal preparation to perform the procedure with confidence. This accessibility could be a game-changer in high-stress environments where delays can be deadly, ensuring that more hands are equipped to act decisively. Additionally, the reduced time to successful intubation means patients receive oxygen faster, lowering the risk of severe complications like brain injury. As a tool that bridges the gap between expertise and urgency, SRIS stands poised to reshape how emergency airway management is approached across various medical fields.
Shaping the Future of Emergency Response
Enhancing Care in Diverse Environments
The potential impact of SRIS on global emergency care is profound, particularly given the millions of intubations performed each year in the U.S. alone, often under challenging circumstances. From roadside trauma scenes to military combat zones and rural clinics with scarce resources, the environments where intubation is needed are rarely ideal. The intuitive nature of SRIS, coupled with its minimal training requirements, could empower a wide array of personnel—paramedics, military medics, and remote clinicians—to secure airways with greater success. By mitigating common complications such as tissue damage and tube misplacement, the device promises improved patient outcomes in settings where traditional tools frequently falter due to stress, poor visibility, or anatomical variability, potentially saving countless lives in the process.
Next Steps Toward Widespread Adoption
While early results are encouraging, the journey of SRIS from prototype to standard medical practice involves critical next steps that must be navigated with care. Clinical trials on live patients are on the horizon to validate the device’s safety and efficacy in real-world conditions, addressing factors like patient comfort that cannot be fully assessed in cadaver studies. Securing FDA approval remains a pivotal milestone, ensuring the system meets rigorous regulatory standards for medical equipment. These phases will determine how soon SRIS can be integrated into hospitals and emergency kits worldwide. As the research team moves forward, the focus will likely remain on refining the technology to handle diverse scenarios and patient needs, paving the way for a future where airway emergencies are managed with unprecedented precision and accessibility.